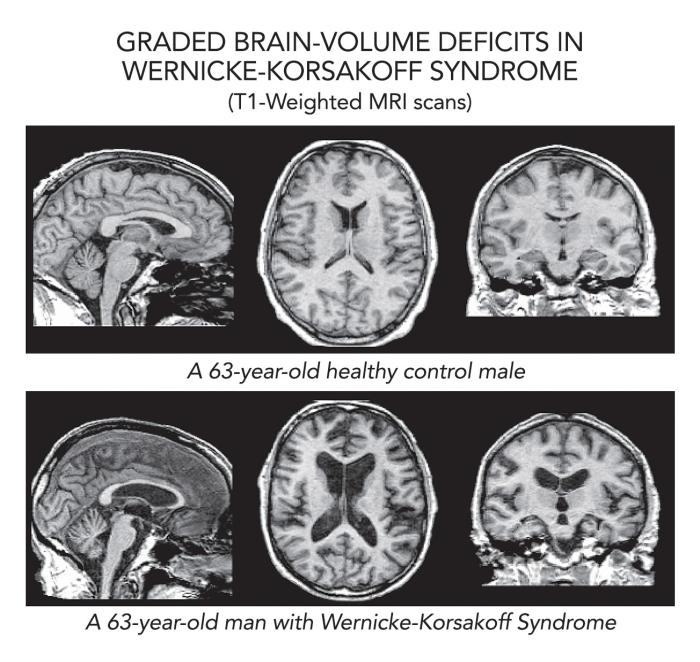
Encephalitis is a buildup of fluid in the brain and can be caused by brain injury, viral infection, certain bacteria, acute organ injury or failure, and, in many cases, chronic alcoholism.
This buildup of fluid is why the disease is commonly called ‘wet brain.’ Treatment options include prompt thiamine (vitamin B1) administration and alcohol cessation, while untreated cases can cause brain damage and create lasting and detrimental memory problems [1] [2] [3].
What Does “Wet Brain” Mean?
“Wet brain” is an informal term for alcohol-related brain damage, most often caused by thiamine (vitamin B1) deficiency. It typically includes two linked conditions—Wernicke encephalopathy and Korsakoff syndrome (WKS).
WKS only happens to people who suffer from end-stage alcoholism. If you occasionally have one or two drinks, you are not at risk for WKS–but that risk increases if you need to drink every day. WKS is preventable, and early diagnosis and treatment can limit permanent disability [1] [2] [3] [4].
What Causes Wet Brain? (Wernicke–Korsakoff & Thiamine Deficiency)
WKS is a life-threatening emergency caused when alcohol interferes with the way your body absorbs, stores, and uses the invaluable antioxidant thiamine (vitamin B1). In the US, most cases of wet brain syndrome are caused by alcohol use disorder (AUD). However, malnutrition from food insecurity or eating disorders, gastrointestinal surgery, or chemotherapy can also cause it, although this is much less common.
Symptoms & Warning Signs
Symptoms of WKS happen in two stages:
- Wernicke encephalopathy
- A transition to Korsakoff syndrome
Symptoms of Wernicke encephalopathy include:
- Confusion
- Eye movement problems
- Ataxia (unsteady gait)
Korsakoff syndrome is a form of severe brain damage. Symptoms include:
- Irreversible memory loss
- Severe anterograde amnesia (the inability to make new memories)
- Confabulation (the creation of false memories) [1] [2] [3] [4].
Source: National Institute on Alcohol Abuse and Alcoholism
Acute Wernicke Encephalopathy: Confusion, Eye Changes, Ataxia
Non-clinical tests for Wernicke Encephalopathy include checking for changes in memory-related mental status, eye “jitters” (nystagmus), eye movement problems or paralysis (ophthalmoplegia), and unsteady gait (ataxia). Not all three must be present, but be aware of the signs [1] [2].
Korsakoff Syndrome: Severe Short-Term Memory Loss & Confabulation
People can seem socially engaged yet have striking memory gaps, repeated questions, and invented explanations to “make sense” of missing memories. Learning new information is especially hard [1] [2] [3].
Is Wet Brain Reversible?
Prompt, high-dose thiamine administered intravenously (IV infusion), often followed by an infusion of glucose, can improve symptoms of wet brain. Supplemental supervised nutrition and hydration will also improve prognosis, but the only way to truly “end” wet brain’s progression is total alcohol cessation and detox from alcohol [1] [2] [3] [4].
If treatment is delayed, WKS can cause permanent brain damage that affects how the brain recalls and creates short-term and long-term memories. Some functions improve with time, nutrition, and cognitive rehab, but full recovery is never guaranteed. Early detox from alcohol is crucial for making a full recovery [1] [2][3] [4] [6].
How Alcohol Leads to Thiamine Deficiency
Poor B1 Intake & Absorption
Alcoholics with end-stage alcoholism will often replace drinking with meals, which reduces the intestine’s ability to absorb vitamins, and increases the body’s need for thiamine.
Impaired Utilization & Liver Disease
Alcoholism damages the liver, where thiamine is stored and metabolized, compounding B1 deficiency [4] [5].
A Dangerous Feedback Loop
Alcoholism reduces the body’s ability to absorb and store thiamine, which in turn increases the body’s need for thiamine. The more vitamin B1 your body loses, the more B1 it needs to get back to normal. Fixing the problem is like paying off a debt with interest, not just replacing what was lost.
Blackouts vs. “Wet Brain” (Not the Same Thing)
Blacking Out Drunk vs. Brownouts
Alcohol-induced blackouts are gaps in memory formation during intoxication (you were awake but didn’t encode memories). Brownouts are a partial recall. These are dose-related events, not the structural memory disorder of Korsakoff syndrome.
Why People Confuse Blackouts With WKS
‘Blacking out’ (drug-related amnesia) is caused by excessive alcohol intake (binge drinking), interfering with the brain’s ability to form short-term memories. WKS is an ongoing (daily) version of being “black-out drunk” but is caused by vitamin deficiency-driven brain damage, not just alcohol abuse alone [1][2][3].
Safer Ways to Stop Drinking: Detox Options & Medications
Alcohol withdrawal can begin 6–24 hours after the last drink; moderate–severe cases can cause seizures or delirium tremens. A clinician can triage you to ambulatory vs. inpatient detox and protect your safety.
Acute alcohol withdrawal is a life-threatening medical condition that happens when alcoholics quit drinking suddenly. It is extremely dangerous to detox alone. If you need to drink every day, seek clinical supervision to complete alcohol detox.
Over-the-Counter vs. Prescription Withdrawal Support
That said, there’s no over-the-counter medicine that “treats” alcohol withdrawal. Common OTC remedies like Alka-Seltzer, aspirin, and other NSAID painkillers may ease minor symptoms of a hangover, but they won’t prevent seizures or delirium caused by alcohol withdrawal. Remember: alcohol withdrawal is not a hangover; it is a life-threatening medical emergency.
Clinician-supervised protocols (e.g., hospitalization, benzodiazepine infusions, tapering off) are standard in some cases to help people quit drinking.
Medicines That Reduce Cravings or Help You Stop Drinking
Evidence-based studies conclude that medications like naltrexone, acamprosate, and disulfiram can reduce alcohol cravings, but only a doctor can prescribe the right one.
Naltrexone, for instance, can be dangerous if self-administered due to its side effects: it blocks the “buzz” caused by alcohol, but it does not stop alcohol’s other effects, like loss of coordination, nausea, and slurred speech. Medication management for alcohol works best in a clinical setting.
Detox and Residential Treatment for Alcohol Addiction in Michigan
Rushton Recovery understands how mental health challenges can be a barrier to recovering from alcohol addiction. Our licensed therapists prioritize your well-being, safety, and comfort throughout treatment. Our detox and residential treatment center in Michigan offers a healing space to embark on your journey toward sobriety.
We offer evidence-based therapies designed to evolve with your individual needs and address the root of your substance abuse. Let our team help you heal, repair relationships, and equip you with the skills to achieve long-term recovery.
Reach out to our Admissions team now.
Sources
- MedlinePlus. (n.d.). Wernicke–Korsakoff syndrome. https://medlineplus.gov/ency/article/000771.htm
- National Institute on Alcohol Abuse and Alcoholism. (n.d.). Wernicke–Korsakoff syndrome. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/wernicke-korsakoff-syndrome
- Wikipedia. (n.d.). Wernicke–Korsakoff syndrome. https://en.wikipedia.org/wiki/Wernicke%E2%80%93Korsakoff_syndrome
- Sechi, G., & Serra, A. (2007). Wernicke’s encephalopathy: New clinical settings and recent advances in diagnosis and management. The Lancet Neurology, 6(5), 442–455. https://pmc.ncbi.nlm.nih.gov/articles/PMC6668891/
- Hoyumpa, A. M. (1980). Mechanisms of thiamin deficiency in chronic alcoholism. The American Journal of Clinical Nutrition, 33(12), 2750–2761. https://pmc.ncbi.nlm.nih.gov/articles/PMC4606320/
- Ceylan, M. F., et al. (2023). Cognitive outcomes after Wernicke encephalopathy: A review. Addictive Behaviors Reports. https://www.sciencedirect.com/science/article/abs/pii/S0306460323000485
- NIAAA. (n.d.). Interrupted memories: Alcohol-induced blackouts. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/interrupted-memories-alcohol-induced-blackouts